Navigating the aftermath of a steroid cycle can feel like a complex puzzle, especially when your body’s natural rhythm seems out of sync. For many athletes and bodybuilders, one of the most disheartening changes is a noticeable dip in libido. This article explores the physiological and psychological factors contributing to decreased sexual desire post-cycle and provides evidence-based strategies to support your recovery.
To understand why libido often falters after a steroid cycle, it is crucial to recognize the significant hormonal shifts occurring within the body. Androgenic-anabolic steroids (AAS) introduce exogenous hormones that suppress the body’s natural hormone production. This suppression impacts the hypothalamic-pituitary-gonadal (HPG) axis, a complex signaling pathway responsible for regulating endogenous testosterone synthesis.
The Role of the HPG Axis
The HPG axis functions as a delicate feedback loop. The hypothalamus releases gonadotropin-releasing hormone (GnRH), which signals the pituitary gland to produce luteinizing hormone (LH) and follicle-stimulating hormone (FSH). LH, in turn, stimulates Leydig cells in the testes to produce testosterone. FSH plays a role in spermatogenesis.
When AAS are introduced, the body perceives an abundance of androgenic hormones. This triggers a negative feedback mechanism, signaling the hypothalamus and pituitary to reduce or cease their production of GnRH, LH, and FSH. Consequently, the testes significantly decrease or halt their natural testosterone production.
The Impact of Suppressed Testosterone on Libido
Testosterone is a primary driver of libido in both men and women, though its precise mechanisms are complex. It influences sexual desire, arousal, and performance. When endogenous testosterone levels are suppressed post-cycle, individuals often experience:
- Reduced sexual desire: A decreased interest in sexual activity.
- Difficulty achieving or maintaining erections: While psychological factors can play a role, physiological testosterone deficiency directly impacts erectile function.
- Reduced pleasure from sexual activity: The overall subjective experience of sex may diminish.
- Fatigue and low energy levels: These are common symptoms of low testosterone and can indirectly affect libido.
The severity and duration of testosterone suppression vary widely depending on the type, dosage, and duration of the steroid cycle, as well as individual physiological responses.
Estrogen Balance and Its Significance
While testosterone is often at the forefront of discussions about male libido, estrogen also plays a critical role. Within the body, testosterone can convert to estrogen via the aromatase enzyme. During and after a steroid cycle, estrogen levels can become imbalanced.
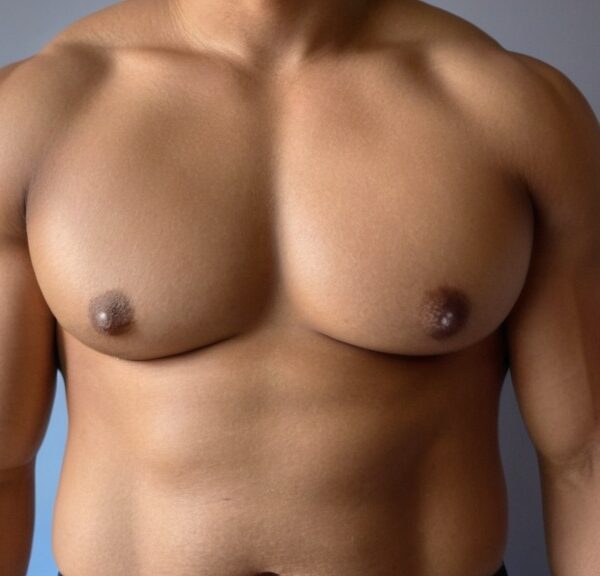
- High estrogen levels: Some AAS aromatize heavily, leading to elevated estrogen. Excess estrogen can paradoxically suppress LH and FSH, further exacerbating low testosterone. It can also cause undesirable side effects like gynecomastia and water retention, which indirectly affect body image and sexual confidence.
- Low estrogen levels: While less common than high estrogen in the immediate post-cycle phase, extremely low estrogen can also negatively impact libido and mood, though its relationship to male sexual function is still an area of ongoing research.
Achieving a healthy testosterone-to-estrogen ratio is crucial for optimal physiological function, including robust libido.
Nutritional Strategies for Hormonal Support
Your diet plays a foundational role in supporting hormonal balance and overall recovery. Think of your body as a high-performance engine; it requires the right fuel to operate efficiently. Specific nutrients contribute to hormone synthesis, neurotransmitter function, and cellular health.
Macronutrient Optimization
- Adequate Protein Intake: Protein provides the amino acids necessary for repairing tissues, synthesizing enzymes, and producing neurotransmitters. Aim for 1.6-2.2 grams of protein per kilogram of body weight from sources like lean meats, poultry, fish, eggs, dairy, and plant-based proteins. Protein is crucial for muscle repair and recovery, which is critical during and after intense training.
- Healthy Fats are Essential: Dietary fats are not merely energy sources; they are precursors to steroid hormones, including testosterone. Prioritize monounsaturated and polyunsaturated fats from avocados, nuts, seeds, olive oil, and fatty fish. Saturated fats in moderation from grass-fed meats or dairy can also contribute to hormone production. Avoid trans fats entirely, as they negatively impact cardiovascular health and hormone function.
- Complex Carbohydrates for Energy and Recovery: Carbohydrates replenish glycogen stores, providing energy for training and aiding in recovery. Opt for complex carbohydrates like whole grains, fruits, and vegetables. These also provide fiber, which supports gut health and nutrient absorption. Sudden and drastic calorie restriction can signal stress to the body, potentially hindering hormone recovery. Maintaining a moderate caloric intake that supports your activity level is important.
Micronutrient Powerhouses
Several vitamins and minerals are directly involved in testosterone production and HPG axis function.
- Zinc: This essential mineral is a cofactor for numerous enzymes involved in hormone synthesis. Studies suggest zinc deficiency can lead to lower testosterone levels. Excellent sources include oysters, red meat, poultry, beans, nuts, and whole grains.
- Magnesium: Involved in over 300 enzymatic reactions, magnesium is crucial for energy production, nerve function, and contributing to free testosterone levels. Leafy green vegetables, nuts, seeds, legumes, and whole grains are rich in magnesium.
- Vitamin D: Often referred to as a “hormone” due to its widespread effects, vitamin D receptors are found in various tissues, including the testes. Research indicates a correlation between adequate vitamin D levels and higher testosterone. Sensible sun exposure and dietary sources like fatty fish, fortified dairy, and supplements can help maintain optimal levels.
- B Vitamins: The B-complex vitamins, particularly B6, B12, and folate, are vital for energy metabolism, nervous system function, and neurotransmitter synthesis, all indirectly supporting hormonal well-being and energy levels crucial for libido.
- Antioxidants (Vitamin C, E, Selenium): Oxidative stress can damage cells and impair hormone production. Antioxidants help protect against this damage. Include a variety of colorful fruits and vegetables in your diet.
The Role of Lifestyle in Recovery

Beyond nutrition, specific lifestyle choices significantly influence your body’s ability to recover hormonal balance and revive libido. These elements work synergistically to create an optimal environment for healing and well-being.
Prioritizing Quality Sleep
Sleep is not merely a period of inactivity; it’s a vital physiological process during which the body repairs, regenerates, and regulates hormones. During deep sleep, the majority of your daily testosterone production occurs, particularly REM sleep.
- Impact of Sleep Deprivation: Chronic sleep deprivation (less than 7-9 hours per night) can significantly lower testosterone levels, increase cortisol (a stress hormone), and negatively affect mood and energy, all contributing to decreased libido.
- Strategies for Better Sleep:
- Consistent Sleep Schedule: Go to bed and wake up at the same time every day, even on weekends.
- Optimize Your Sleep Environment: Ensure your bedroom is dark, quiet, and cool.
- Limit Screen Time: Avoid electronic devices emitting blue light for at least an hour before bed.
- Avoid Caffeine and Alcohol: Especially close to bedtime, as they disrupt sleep architecture.
- Relaxation Techniques: Incorporate winding-down rituals like reading, a warm bath, or meditation.
Managing Stress Effectively
Stress, whether physical or psychological, triggers the release of cortisol from the adrenal glands. While cortisol is essential for acute stress responses, chronically elevated levels can suppress testosterone production. The body prioritizes survival over reproduction when under constant stress.
- Impact of Chronic Stress: Long-term stress not only directly suppresses testosterone but also impacts mood, energy levels, and overall mental well-being, all of which are intricately linked to libido.
- Stress Reduction Techniques:
- Mindfulness and Meditation: Practicing mindfulness can reduce cortisol levels and improve emotional regulation.
- Deep Breathing Exercises: Simple techniques can calm the nervous system.
- Regular Physical Activity: While intense training can be a stressor, moderate exercise is a powerful stress reliever.
- Hobbies and Social Connection: Engage in activities you enjoy and maintain strong social bonds.
- Time Management: Organizing your daily tasks can reduce feelings of overwhelm.
The Importance of Consistent, Moderate Exercise
While your training intensity might have been extreme during a cycle, post-cycle recovery requires a thoughtful approach to exercise.
- Avoid Overtraining: Excessive training post-cycle can be counterproductive. It acts as a physical stressor, potentially elevating cortisol and hindering hormonal recovery.
- Focus on Strength Training: Continue lifting weights, but adjust volume and intensity downwards initially. Strength training has been shown to acutely increase testosterone levels and maintain muscle mass during recovery.
- Incorporate Cardiovascular Exercise: Moderate cardio improves cardiovascular health, reduces stress, and aids overall well-being.
- Listen to Your Body: Pay attention to signs of fatigue, persistent soreness, or mood changes, and adjust your training accordingly.
Therapeutic Approaches and Considerations

While lifestyle and nutrition form the bedrock of recovery, some individuals may benefit from targeted therapeutic approaches to accelerate hormonal restoration and address persistent low libido.
Post-Cycle Therapy (PCT) Considerations
Post-Cycle Therapy (PCT) aims to restore natural testosterone production and mitigate estrogenic side effects after an anabolic steroid cycle. It often involves the use of specific pharmaceutical compounds.
- Selective Estrogen Receptor Modulators (SERMs): Compounds like tamoxifen (Nolvadex) and clomiphene (Clomid) are commonly used in PCT. They work by blocking estrogen receptors in the hypothalamus and pituitary, thereby reducing estrogen’s negative feedback on the HPG axis. This prompts the pituitary to increase LH and FSH production, stimulating endogenous testosterone synthesis in the testes.
- Clomiphene: Known for its ability to stimulate LH and FSH, it effectively helps kickstart natural testosterone production. Some individuals report visual disturbances or mood swings as side effects.
- Tamoxifen: Also blocks estrogen receptors and is often used alongside clomiphene or for specific estrogen-related side effects like gynecomastia.
- Aromatase Inhibitors (AIs): Medications like anastrozole (Arimidex) or exemestane (Aromasin) prevent the conversion of testosterone to estrogen. While sometimes used during a cycle to manage high estrogen, their use post-cycle requires careful consideration. Excessive lowering of estrogen can also negatively impact libido and bone density. Close monitoring of estrogen levels is essential if considering an AI during PCT.
- Human Chorionic Gonadotropin (hCG): hCG mimics LH and can directly stimulate Leydig cells in the testes to produce testosterone. It is often used during longer cycles or when significant testicular atrophy has occurred, to maintain testicular function and size, making recovery smoother. It is generally not used alone for PCT but rather as a bridge during or immediately after a cycle, before initiating SERMs.
Important Note: The use of PCT medications should always be under the guidance of a qualified medical professional. Self-prescribing can lead to suboptimal outcomes, further hormonal imbalances, or adverse side effects. A healthcare provider can assess your individual needs through blood work and create a safe and effective recovery plan.
Addressing Psychological Factors
Libido is not solely a physiological phenomenon; it is deeply intertwined with psychological well-being. Post-cycle, many individuals experience mood disturbances, anxiety, or depression, all of which can severely impact sexual desire.
- Mood Fluctuations: The rapid decline in testosterone levels post-cycle can mimic symptoms of hypogonadism, including irritability, mood swings, and general malaise. These emotional changes can diminish interest in sex.
- Body Image Concerns: While steroids can enhance physique, the fear of losing gains or changes in body composition post-cycle can lead to body image dissatisfaction and self-consciousness, directly impacting sexual confidence.
- Performance Anxiety: Concerns about sexual performance, often rooted in past experiences or fear of not meeting expectations, can create a self-fulfilling prophecy, making arousal and enjoyment difficult.
- Coping Mechanisms:
- Counseling or Therapy: A mental health professional can help process these emotions, develop coping strategies, and address underlying psychological barriers to sexual health. Cognitive Behavioral Therapy (CBT) can be particularly effective.
- Mindfulness and Stress Reduction: As mentioned previously, these practices can improve emotional regulation and reduce anxiety.
- Open Communication with Partners: Discussing feelings and fears openly with a sexual partner can alleviate pressure and foster understanding.
- Focus on Overall Well-being: Engage in activities that bring joy and a sense of accomplishment outside of physical appearance or athletic performance.
When to Seek Professional Medical Advice
While the strategies outlined in this article can significantly aid recovery, there are instances when consulting a medical professional is imperative.
- Persistent Low Libido: If low libido persists for several months despite adhering to lifestyle changes and a PCT protocol, further medical investigation is warranted.
- Severe Mood Disturbances: Intense depression, anxiety, panic attacks, or thoughts of self-harm require immediate professional intervention.
- Erectile Dysfunction: Persistent inability to achieve or maintain an erection should be evaluated by a urologist or endocrinologist.
- Changes in Testicular Size or Consistency: These symptoms could indicate ongoing testicular dysfunction.
- Abnormal Blood Work: If follow-up blood tests show continued low testosterone, high estrogen, or other significant hormonal imbalances, a physician can adjust treatment.
A qualified healthcare provider can conduct comprehensive blood tests (including total and free testosterone, LH, FSH, estradiol, prolactin, SHBG), assess your individual health profile, and rule out other potential causes for your symptoms. They can then recommend appropriate interventions, which may include further pharmaceutical support, optimizing existing PCT, or exploring other therapeutic avenues. Your health is a long-term investment, and professional guidance ensures the safest and most effective recovery journey.
Embracing a Holistic Recovery Process
| Metric | Description | Typical Range | Notes |
|---|---|---|---|
| Libido Level | Subjective measure of sexual desire post cycle | Low to High (1-10 scale) | Often reduced immediately after cycle, may recover over weeks |
| Testosterone Levels | Serum testosterone concentration | 300-1000 ng/dL (normal range) | May be suppressed post cycle, impacting libido |
| Luteinizing Hormone (LH) | Hormone stimulating testosterone production | 1.5-9.3 IU/L | Suppressed during cycle, recovery important for libido restoration |
| Follicle Stimulating Hormone (FSH) | Hormone involved in reproductive function | 1.4-18.1 IU/L | Levels may be low post cycle, affecting libido indirectly |
| Estradiol Levels | Estrogen hormone level | 10-40 pg/mL | Imbalance can affect libido and mood post cycle |
| Recovery Time | Time taken for libido to return to baseline | 2-12 weeks | Varies based on individual and post cycle therapy |
Returning to optimal health and sexual well-being after a steroid cycle is not a singular event but a continuous journey. It requires patience, consistency, and a multi-faceted approach that addresses physiological, nutritional, and psychological components.
Patience and Realistic Expectations
The body’s endocrine system is complex, and its recovery does not happen overnight. Just as it took time for suppression to occur, it will take time for the HPG axis to fully regain its natural rhythm. Hormonal recovery often spans several weeks to many months, and in some cases, can be longer.
- Setting Realistic Timelines: Understand that you may not feel 100% instantly. Celebrate small improvements and acknowledge that fluctuations in mood and energy are normal during this transitional period.
- Avoiding Quick Fixes: Resist the temptation to jump into another cycle or resort to unproven remedies. These can often exacerbate existing issues and derail your recovery progress.
- Focus on Process, Not Just Outcome: Concentrate on consistently applying the positive lifestyle and nutritional strategies discussed. The outcome will follow the process.
The Power of Positivity and Self-Compassion
The recovery period can be challenging, not just physically but emotionally. It is crucial to cultivate a positive mindset and practice self-compassion.
- Acknowledge Your Efforts: Recognize the effort you are putting into your recovery. It is a sign of strength and commitment to your long-term health.
- Avoid Self-Criticism: It is easy to become frustrated when progress feels slow or when libido remains lower than desired. Be kind to yourself. Understand that your body is undergoing significant adjustments.
- Focus on Overall Well-being: Shift your focus from solely physical performance or appearance to a broader definition of health, encompassing mental clarity, emotional balance, and energy levels. These contribute significantly to a fulfilling life, including a healthy sex life.
Long-Term Health and Sustainability
This recovery phase is an opportunity to re-evaluate your approach to health and fitness, prioritizing sustainable practices that support longevity and well-being.
- Building Sustainable Habits: The nutritional and lifestyle strategies outlined (quality sleep, stress management, balanced diet, moderate exercise) are not just for post-cycle recovery; they are fundamental for lifelong health.
- Regular Health Check-ups: Establish a routine of regular medical check-ups, including comprehensive blood work, even after you feel fully recovered. This helps monitor long-term hormonal health and detect any potential issues early.
- Educate Yourself: Continue learning about your body, its functions, and ways to support its optimal health naturally. Knowledge empowers you to make informed decisions.
- Redefine Success: Explore what “success” means to you beyond absolute strength or muscle mass. A fulfilling life includes vibrant health, strong relationships, and robust well-being, of which a healthy libido is a component.
Reviving your libido after a steroid cycle requires a methodical and patient approach. By proactively addressing hormonal imbalances, optimizing nutrition, embracing healthy lifestyle choices, and seeking professional guidance when needed, you can successfully navigate this recovery phase and restore not only your sexual desire but also your overall vitality and zest for life. Your journey is unique, and by prioritizing your holistic well-being, you pave the way for a healthier, more balanced future.
FAQs
What is post cycle libido?
Post cycle libido refers to the changes in sexual desire and function that occur after completing a cycle of anabolic steroids or other performance-enhancing drugs. It is common for individuals to experience a decrease in libido during the post cycle period due to hormonal imbalances.
Why does libido decrease after a steroid cycle?
Libido decreases after a steroid cycle because the body’s natural testosterone production is suppressed during steroid use. When the cycle ends, it takes time for the body to restore normal hormone levels, leading to reduced sexual desire and function temporarily.
How long does it take for libido to return to normal post cycle?
The time it takes for libido to return to normal varies depending on the individual, the length and dosage of the steroid cycle, and whether post cycle therapy (PCT) is used. Generally, it can take anywhere from a few weeks to several months for hormone levels and libido to fully recover.
What is post cycle therapy (PCT) and how does it affect libido?
Post cycle therapy (PCT) involves using medications such as selective estrogen receptor modulators (SERMs) or human chorionic gonadotropin (hCG) to help restore natural testosterone production after a steroid cycle. Effective PCT can significantly reduce the duration and severity of post cycle libido loss.
Can lifestyle changes help improve post cycle libido?
Yes, lifestyle changes such as maintaining a balanced diet, regular exercise, adequate sleep, stress management, and avoiding alcohol or recreational drugs can support hormonal recovery and improve libido after a steroid cycle. Consulting a healthcare professional is also recommended for personalized advice.